What is Tranq?
What is tranq, and what makes it so dangerous?
Tranq is a mixture of fentanyl, the potent opioid, plus xylazine, an animal tranquilizer. It’s dangerous for a few reasons.
First, it’s a powerful sedative and can leave users unconscious for hours. For people who use drugs outdoors or alone, this can be a risky situation.
Second, its presence in the drug supply can’t be easily detected. Fentanyl test strips, for example, are a reliable way for drug users and researchers to see if a given drug sample is tainted with fentanyl. Right now, no such resource exists to detect tranq.
Third, overdoses that involve tranq are more complex — and potentially more deadly.
Does naloxone, or Narcan, work on tranq overdoses?
Yes. But it will be less effective than it is in more traditional opioid overdose cases.
“Xylazine, to our knowledge, does not respond to naloxone, but the opioids that are almost always present with the xylazine will respond to it. And what you want to do is give that person the opportunity to breathe,” Jen Shinefeld, an epidemiologist with the City of Philadelphia’s Department of Public Health, told VICE News.
Other elements of overdose rescue are especially essential when tranq is involved.
What should you do if someone is overdosing on tranq?
- Call 911
- Administer naloxone
- Begin rescue breathing
- If/when breathing resumes, roll the person into the recovery position
What other complications does tranq present?
The biggest risk, after overdose, is serious wounds. Harm reduction groups and doctors report that tranq use seems to cause painful skin lesions and sores that rapidly get worse. Wounds like this are typically only a risk for injection drug users — but experts say that even people who smoke or snort tranq are at-risk for dangerous sores that can quickly get infected if left untreated.
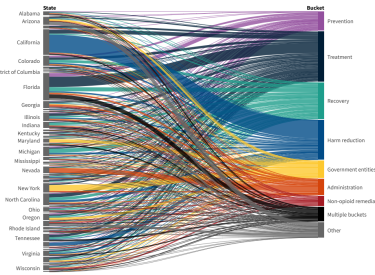
Where is tranq showing up in the U.S. drug supply?
It first appeared in Philadelphia, but is quickly emerging in the street supply of drugs in cities across the country, from Chicago to Texas, according to STAT News.
Stigma can get in the way of effective treatment.
“A concern is that people who use drugs — because they are often treated poorly by medical providers — won’t seek help for their wounds until they’ve advanced to a dangerous point,” STAT reports.
Stigma is always a big barrier to addiction treatment and recovery, and its effect is even more powerful when a new, lesser understood drug emerges within the street supply.
When using a new substance like tranq, people may not understand the risks and side effects, or they may be embarrassed by their symptoms, preventing them from seeking care.
Medical professionals who aren’t aware of the emerging drug, or who aren’t used to treating patients who use drugs, will not be able to care for these patients effectively. That’s why sharing accurate, useful information about the outbreak is so critical.
There are a lot of unknowns. But experts are working on solutions.
Though no test strip exists to detect tranq, researchers have been able to follow its spread by studying regional outbreaks of wounds and skin issues.
Researchers are trying to understand what exactly is causing the wounds associated with tranq use. They’re also exploring how tranq impacts overdoses. Is xylazine itself impacting a user’s breathing? Or is it still mainly the opioids present in the drug cocktail that put people at risk of fatal overdose?
Meanwhile, local harm reduction groups are exploring new ways to help people survive tranq overdoses, like administering oxygen after a person’s been revived.
Though the emergence of potent new drugs can be scary, it’s important to remember that science-based addiction treatment is highly effective and opioid-involved overdoses are still reversible with the right know-how. Learn more about addiction treatment and overdose safety.